A blood transfusion is needed for low hemoglobin when other treatments have been ineffective in increasing the levels of hemoglobin in the body. Low hemoglobin can lead to symptoms such as fatigue, weakness, and shortness of breath, and a blood transfusion can help to replenish the levels of hemoglobin and improve these symptoms.
Low hemoglobin, or anemia, is a condition that occurs when there is a decreased level of hemoglobin in the blood. Hemoglobin is a protein found in red blood cells that helps transport oxygen from the lungs to the rest of the body.
When hemoglobin levels are low, the body may not be receiving enough oxygen, leading to symptoms such as fatigue, weakness, and shortness of breath. While there are various treatments available for low hemoglobin, such as dietary changes, supplements, and medications, a blood transfusion may be necessary when these methods do not effectively increase hemoglobin levels. We will explore when a blood transfusion is needed for low hemoglobin and why it is an important treatment option.
Credit: www.drrpadmakumar.com
Understanding Hemoglobin And Its Importance
A blood transfusion may be necessary when a person has low hemoglobin levels. Hemoglobin plays a vital role in carrying oxygen throughout the body, and a low level can lead to various health issues. Understanding the importance of hemoglobin helps to determine when a blood transfusion is needed.
What Is Hemoglobin?
Hemoglobin is a protein found in our red blood cells that plays a vital role in our body. It is responsible for transporting oxygen from the lungs to different parts of the body and carrying carbon dioxide back to the lungs to be exhaled. Without hemoglobin, our body would not be able to function properly.
The Role Of Hemoglobin In The Body
Hemoglobin plays a crucial role in maintaining the health and well-being of our body. It ensures that every cell in our body receives the oxygen it needs to carry out various functions. Here’s a closer look at the main functions of hemoglobin:
- Transporting Oxygen: Hemoglobin binds with oxygen in the lungs and forms a complex, known as oxyhemoglobin. This complex is then carried through the bloodstream to all parts of the body, where it releases oxygen to sustain cellular activities.
- Removing Carbon Dioxide: Hemoglobin also helps in removing carbon dioxide, which is a waste product generated by our cells. It picks up carbon dioxide from tissues and transports it to the lungs for elimination.
- Maintaining pH Balance: Hemoglobin plays a crucial role in maintaining the pH balance of our body fluids. It acts as a buffer, preventing significant changes in pH levels, which can be harmful to our cells and overall bodily function.
- Regulating Blood Flow: Hemoglobin helps regulate blood flow by expanding or contracting blood vessels as per the oxygen requirements of different tissues. This ensures an adequate supply of oxygen to all parts of the body.
- Supporting Cellular Metabolism: Cellular metabolism requires a constant supply of oxygen to produce energy. Hemoglobin ensures that oxygen reaches the cells efficiently, promoting proper metabolism and overall cell function.
Considering the vital role that hemoglobin plays in our body, it becomes crucial to ensure its levels are within normal range. When the hemoglobin levels drop significantly, it may lead to a condition called anemia, which can result in various symptoms like fatigue, shortness of breath, and pale skin. In such cases, a blood transfusion may be needed to replenish the hemoglobin levels and restore the body’s oxygen-carrying capacity.
Now that we understand the importance of hemoglobin and how it functions in our body, let’s delve deeper into when a blood transfusion is required for low hemoglobin levels.

Credit: www.sciencedirect.com
Causes And Symptoms Of Low Hemoglobin
Low hemoglobin levels can be caused by a variety of factors and can lead to serious health issues if not addressed promptly. In this section, we will explore the common causes and signs of low hemoglobin, giving you a better understanding of when a blood transfusion may be necessary.
Common Causes Of Low Hemoglobin Levels
Several common causes can contribute to low hemoglobin levels in the body:
- Blood loss: Whether from an injury, surgery, or internal bleeding, excessive blood loss can lower hemoglobin levels. This can occur due to accidents, gastrointestinal bleeding, or heavy menstrual periods.
- Dietary deficiencies: Inadequate intake of essential nutrients like iron, vitamin B12, and folate can lead to low hemoglobin levels. These nutrients are required for the production of healthy red blood cells.
- Chronic diseases: Certain chronic conditions, such as kidney disease, liver disease, and cancer, can affect the body’s ability to produce and maintain a healthy level of hemoglobin.
- Anemia: Anemia is a condition characterized by low hemoglobin levels. It can be caused by various factors, including iron deficiency, vitamin deficiencies, and certain chronic diseases.
Signs And Symptoms Of Low Hemoglobin
Recognizing the signs and symptoms of low hemoglobin is crucial for early detection and appropriate treatment. Here are some common indicators to watch out for:
- Weakness and fatigue: Feeling constantly tired or weak, even after sufficient rest, can be a sign of low hemoglobin levels.
- Shortness of breath: If you find yourself out of breath with minimal physical activity, it may be due to inadequate oxygen-carrying capacity in the blood caused by low hemoglobin.
- Dizziness and lightheadedness: Low hemoglobin levels can lead to insufficient blood flow to the brain, resulting in dizziness and a feeling of lightheadedness.
- Pale skin and nail beds: Reduced hemoglobin levels can lead to paleness in the skin and nail beds.
- Rapid or irregular heartbeat: Anemia-related low hemoglobin can cause the heart to work harder to pump oxygen-rich blood to the body, resulting in an increased heart rate or irregular heart rhythm.
Understanding the common causes and recognizing the signs and symptoms of low hemoglobin can help you assess when a blood transfusion may be needed. If you experience any of these symptoms or suspect low hemoglobin levels, it is important to consult a healthcare professional for proper diagnosis and treatment.
Diagnosing And Monitoring Low Hemoglobin
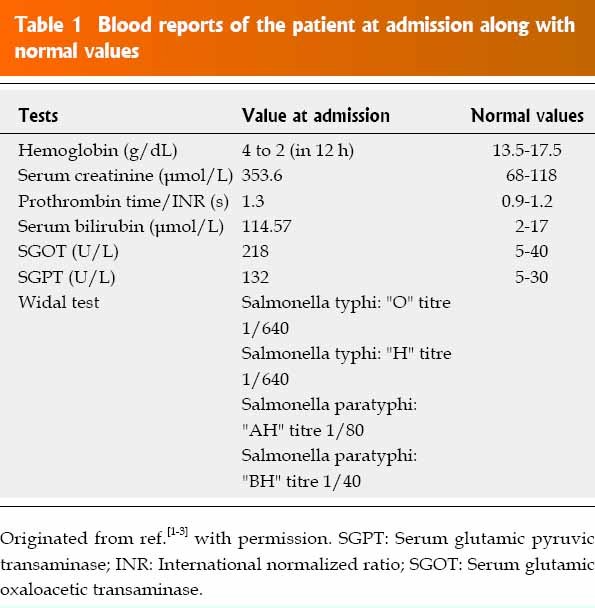
When it comes to diagnosing and monitoring low hemoglobin levels, several tests can provide valuable insights and help ensure proper treatment. By detecting low hemoglobin levels early on, medical professionals can determine the need for a blood transfusion and contain more serious complications. Regular monitoring of hemoglobin levels is also essential to track progress and adjust treatment plans accordingly.
Tests To Diagnose Low Hemoglobin
Diagnosing low hemoglobin begins with a thorough medical evaluation, where doctors may ask about symptoms, medical history, and any recent blood loss. Blood tests are then conducted to measure hemoglobin levels accurately. These tests may include:
- The Complete Blood Count (CBC) test, measures red blood cell count, hemoglobin level, hematocrit level, and other blood components.
- The Iron Panel evaluates iron levels in the blood and determines if an iron deficiency is causing low hemoglobin.
- The Reticulocyte Count, which checks the production and release of immature red blood cells, a sign of bone marrow activity.
- The Serum Ferritin Test, measures the level of ferritin in the blood, a protein that stores iron.
Based on the results of these tests, doctors can determine the underlying cause of low hemoglobin and plan the appropriate course of treatment, which may or may not include a blood transfusion.
Monitoring Hemoglobin Levels Over Time
After the initial diagnosis, it is crucial to regularly monitor hemoglobin levels to ensure the effectiveness of the treatment plan. By closely tracking these levels, doctors can make necessary adjustments and evaluate the progress of the patient’s condition. Common methods for monitoring hemoglobin levels include:
- Periodic blood tests that measure hemoglobin levels and provide updated information on the patient’s condition.
- Visual examination of symptoms and signs of anemia, such as fatigue, pale skin, and shortness of breath.
- Monitoring other blood parameters, such as red blood cell count and hematocrit levels, to gain a comprehensive understanding of the patient’s blood health.
Regular monitoring ensures that any significant changes in hemoglobin levels are promptly identified and addressed. This allows medical professionals to determine if a blood transfusion is needed or if alternative treatments can be pursued to increase hemoglobin levels naturally. Effective monitoring is vital for managing low hemoglobin and reducing the risk of complications.

Credit: www.the-hospitalist.org
When Is A Blood Transfusion Needed For Low Hemoglobin
Low hemoglobin levels can be a cause for concern and may require a blood transfusion in certain cases. Hemoglobin is a protein found in red blood cells that carries oxygen throughout the body. When the hemoglobin level falls below a certain threshold, it can lead to symptoms like fatigue, shortness of breath, and weakness.
Criteria For Blood Transfusion
A blood transfusion is typically recommended when a patient’s hemoglobin level drops to a specific point, known as the transfusion threshold. The decision to administer a blood transfusion is based on several factors, including:
- The severity of symptoms: If the low hemoglobin levels are causing significant symptoms and impairing the patient’s quality of life, a blood transfusion may be necessary to alleviate these symptoms and improve the patient’s well-being.
- The underlying cause: The cause of low hemoglobin levels also plays a role in determining the need for a blood transfusion. Some conditions, such as acute bleeding or severe anemia, require immediate replenishment of red blood cells through transfusion.
- Trends in hemoglobin levels: The rate at which hemoglobin levels are declining can also influence the decision for a blood transfusion. If the levels are rapidly dropping, it suggests an acute problem that may require urgent intervention.
Risks And Benefits Of Blood Transfusion
While blood transfusions can be life-saving in certain situations, they are not without risks. It is important to weigh the potential benefits against the possible complications. Some of the risks associated with blood transfusions include:
- Allergic reactions: Some individuals may experience an allergic reaction to the transfused blood, leading to symptoms like itching, hives, or difficulty breathing.
- Transfusion-related infections: Although the risk is minimal due to extensive testing, there is a small possibility of acquiring an infection from the donor blood.
- Transfusion-related lung injury: In rare cases, transfusions can cause lung damage, resulting in difficulty breathing and low oxygen levels.
- Overload of iron: Frequent blood transfusions can lead to a buildup of iron in the body, which may require additional treatment to manage.
Despite the potential risks, blood transfusions are vital in certain situations and can provide immediate relief to individuals with low hemoglobin levels. The decision to proceed with a blood transfusion should always be made in consultation with a healthcare professional who can assess the patient’s specific circumstances and determine the most suitable course of action.
Frequently Asked Questions For When Is A Blood Transfusion Needed For Low Hemoglobin
Q: How Do You Know If You Need A Blood Transfusion For Low Hemoglobin?
A: If you experience fatigue, dizziness, and shortness of breath, along with low hemoglobin levels, a blood transfusion may be necessary.
Q: What Is Considered A Low Hemoglobin Level That Requires A Blood Transfusion?
A: Hemoglobin levels below 70 g/L for adults or below 90 g/L for children are generally considered low enough to require a blood transfusion.
Q: What Are The Benefits Of A Blood Transfusion For Low Hemoglobin?
A: A blood transfusion can improve oxygen delivery to tissues, alleviate symptoms like weakness and fatigue, and prevent complications associated with low hemoglobin levels.
Conclusion
A blood transfusion is often necessary when a person’s hemoglobin levels drop significantly. By replenishing red blood cells, this procedure helps improve oxygen transport and overall health. It is crucial to monitor symptoms such as fatigue, shortness of breath, and pale skin to determine the need for a blood transfusion.
Early intervention and proper medical guidance are essential for effective treatment. Remember, your well-being is a priority, and seeking medical advice is crucial when experiencing low hemoglobin levels.
